1
HIGH
DEFAULTER RATE AMONG PATIENTS WITH CHRONIC DISEASES
IN THE HEALTH
CLINICS IN THE DISTRICT OF PENDANG, 2003
Dr.
Hjh Hayati Mohd Radzi1, Dr.Hjh Baizury Bashah2,Dr.Loh
Leh Teng 3,
KJK
Ishah Rashid4, JK Julita Md Zain5, PP Azman
Ibrahim6, JK Zurina Che Ani7, PP Hussein
Abdul Rahim8, JK Radziah Talib9, PP Zainol
Man10.
1.
OUTLINE OF THE PROBLEM
Defaulters
among patients with chronic diseases from the appointment date for
follow-up is of great
concern to the service providers. This is because if the problem
is not addressed effectively and efficiently, it will result in
uncontrolled disease conditions and complications which may lead
to high morbidity and mortality. Chronic diseases are defined as
lifestyle diseases such as diabetes, hypertension and
cardiovascular disease or diseases that require long term
treatment such as asthma, epilepsy or psychiatric conditions.
The
district quality committee members had a meeting to identify
quality problems in the district. Nominal group techinique was
used to identify the problems and voting was done using the SMART
criteria to prioritise the problem. The problem with the highest
score was chosen as the problem which needed immediate attention.
The problem chosen was the high defaulter rate among patients with
chronic diseases in the health clinics in the district of Pendang.
A
verification study was carried out in all the three health
clinics. The card study involving all the patients with chronic
diseases was reviewed for two months in 2002. It was noted that
the defaulter rate averaged at 24.3% for all the three clinics.
Better compliance to clinic appointment among patients with
chronic disease will improve disease control, better compliance to
treatment and hence
improve the quality of life. Shortage of medication given to
patients may result in self-adjusting the dosage to cover for the
missed appointment or by buying the medication off the counter at
pharmacies. This condition may result in uncontrolled diabetes,
severe hypertension, unstable angina, status asthmaticus or
epileptic seizures.
The
reasons for defaulting may be due to weaknesses in the patient’s
management system, ineffective health education, problems to keep
to the appointment given and the patients’ attitude.
Some
remedial measures that hope to be implemented are to put in place
such as a defaulter tracing system, reminders for the frequent
defaulters, scheduled health education sessions on their disease
condition and to create appointment books for doctors and medical
assistants. It is hoped that with the implementation of the
remedial measures the defaulter rate will reduce, thus increasing
the knowledge of patients and promoting the healthy lifestyle.
2.
KEY MEASURES FOR IMPROVEMENT
The
indicator chosen to indicate improvement in the defaulter rate is
the percentage of patients with chronic disease complying to the
appointment date given. The standard set was 15%. The standard set
was due to an earlier study that showed that only 40% of the
reasons for defaulting are remediable.
A
model of good care was set in accordance to the management of
patients with chronic diseases based on Clinical Practise
Guideline issued by the Ministry of Health. The processes chosen
for the model of good care were the appointment date given,
reminders for patients identified as high risk of defaulting,
knowledge of patients on their diseases, scheduled health
education sessions on the various topics of their disease and
defaulter tracing for those who default from the appointment date.
Standards and criterias were set for each process. Achievements
were measured before and after the remedial measures done. The
achievements were monitored monthly.
3.
PROCESS OF GATHERING INFORMATION
Data
were gathered to identify the reasons for defaulting and the
patients’ knowledge on
disease. A systematic random sampling was used to sampel the
defaulters to ascertain the reasons for defaulting. A pretest
questionnaire was designed and the patients were interviewed by
trained interviewers. A total of 200 defaulters
were sampled for the month of March, 2003.
4.
ANALYSIS AND INTERPRETATIONS
The
data collected were analysed using the Epi Info version 6.04. The
findings for the reasons for defaulting were forgot the
appointment date, was away from home/district, transportation
problems, medication still available and others. 92.6% of those
who defaulted will come back to the clinic in less than 2 weeks of
defaulting. Only 83.8% had complete addresses on the OPD cards and
only 51.3% had telephone numbers written on their treatment cards.
About 75% had health education sessions about their disease but
only 20.8% of patients had good knowledge (patients with score of
more than 75%) on their disease. Moreover there is not much
increase in their lifestyle pattern. Diet intake showed good
practice of taking balanced,
nutritious and appropriate food for their disease condition.
5.
STRATEGY FOR CHANGE
Strategies
carried out to improve the defaulter rate were to improve on the
health education sessions, improve on the defaulter tracing
system, reminder for those high risk of defaulting, complete
information of patients to assist in defaulter tracing and
improving the knowledge of patients on their disease conditions.
Information of patients are updated which included address and
telephone number (neighbours, friends etc). Defaulter tracing
system was reinforced, patients who do not come after the clinic
sessions will be identified and reminders will be sent via letters
or they will be contacted if telephone numbers were available.
Health education sessions were scheduled and health educations
materials were made to assist the staffs. The health education
contents stressed on facts about the chronic diseases, medication,
quit smoking, eat healthy, exercise and complications of the
disease etc. Those with high risk of defaulting will be identified
using a checklist and will be tagged with a black thread. The will
be called to remind of the appointment date or given letters of
reminder.
6.
EFFECTS OF CHANGE
After
3 months of implementation of the remedial measures, the defaulter
rate has improved from 24.3% to 16%. There is a reduction in ABNA
from 8.3% to 1% after implementation of remedial measures. The
processes and standards in the model of good care were monitored
monthly. After 3 months, an evaluation study was carried out. The
complete information about patient has improved at 83.8%. Patients
given appointment date has improved from 98.3% to 100%. High risk
patients given reminders on their appointment date has improved
from 0% to 85.7%. With the implementation of scheduled health
education sessions (33.3% to 100%) the knowledge of patients had
improved from 20.8% to 42%. Defaulter tracing has improved from 0%
to 81.5%.
7.
THE NEXT STEP
From
this project, it has shown that integrated and holistic approach
to implementing the remedial measures has shown tremendous
improvement in the management of the patients. The involvement of
nursing staff in health education has managed to scheduled the
health education session and managed to improve the knowledge of
patients by 20%. The defaulter tracing system was now in place and
became part of the whole patient’s management system in the
health clinics. The next step will be to improve in the control of
the individual diseases such as control of diabetes, control of
hypertension etc. because it is closely related to improving their
quality of life and hence being able to reduce the complication of
the disease.
1
Medical Officer of Health, 2 Family Medicine Specialist, 3 Medical
and Health Officer, 4 Health Sister, 5 Staff Nurse, Pendang HC, 6
Medical Assistant Pendang HC, 7 Staff Nurse Sg. Tiang HC, 8
Medical Assistant Sg. Tiang HC, 9 Staff Nurse Kubur Panjang HC, 10
Medical Assistant Kubur Panjang HC
ABSTRACT
HIGH
DEFAULTER RATE AMONG PATIENTS WITH CHRONIC DISEASES IN THE HEALTH
CLINICS IN THE DISTRICT OF PENDANG, 2003
Dr.
Hjh Hayati Mohd Radzi1, Dr.Hjh Baizury Bashah2,Dr.Loh
Leh Teng 3,
KJK
Ishah Rashid4, JK Julita Md Zain5, PP Azman
Ibrahim6, JK Zurina Che Ani7, PP Hussein
Abdul Rahim8, JK Radziah Talib9, PP Zainol
Man10
Chronic
diseases such as diabetes , hypertension and cardiovascular
disease or diseases that required long term treatment such as
asthma , epilepsy or psychosis conditions are
defined as lifestyle diseases.
Defaulters among these patients with chronic diseases from
the appointment date for follow-up is of great concern to the
service providers If
this problem is not addressed effectively and efficiently it will
lead to uncontrolled disease conditions and complications
which may result to high morbidity and mortality.
A
verification study was carried out in
all the three health clinics in the district of Pendang
among the patients with chronic diseases. The
finding shows that 28%
among the patients with chronic diseases defaulted their
apppointments and hence also defaulted their treatments .
Monitoring
indicators and standards were set. The indicator is the percentage
of patient with chronic disease that defaulted their apponitment
date and the standard set is 15%.
This standard was set following an earlier study showed that 40%
of reasons of defaulting can
be overcome by
remedial actions. A system
of defaulter tracing
was introduced, all chronic cases that come for treatment are
registered, registration books are kept by doctors or Medical
Assistants that treat the patient so as to ensure all defaulters
can trace when appointment dates are given to them.
After 3 months of implementing the remedial measures, the restudy showed
there is an increase in knowledge
among patients with more than 75% score knowledge on their
disease from 29.7% to 42%.
Defaulter rate decreased from 28.8% to 15.8%.
***************************************************************************
POOR COVERAGE OF OPV/DPT BOOSTER AMONG
TODDLERS
IN DISTRICT OF PENDANG, KEDAH
Hayati Md. Radzi, Baizury Bashah, Maimunah
Md. Noor, Ishah Rashid, Salihah Hashim, Azizah Ramli, Che Olah
Zakaria
- ABSTRACT
The
poor coverage of OPV/DPT booster among toddlers was identified as
a quality problem following the district quality committee
meeting. The project was selected thorough the nominal group
technique using the SMART criteria. The booster coverage for
toddler was low, achieving 60.9% in 2002. Toddler attendances was
only 33.3% (2586) in 2002. Booster immunization is important to
maintain optimal antibody level against immunisable diseases
before another dose of DT/Polio booster is given in Std 1. Poor
coverage of immunization may increase the child’s susceptibility
to immunisable diseases.
The indicator
choosen was coverage of booster immunization and the standard set
was at 95%. A survey on knowledge of mothers on immunization noted
that only 11.1% obtained at score of > 75% and as a whole still
poor in knowledge about immunization and its importance. A model
of good care was designed. Among the strategies for change were
filing of cards according to completion of immunization, defaulter
tracing, monthly monitoring of immunization achievement, missed
opportunities, health education to staffs and mothers, assessment
of toddlers, supervision and activities for toddlers.
The strategies
for change were implemented for 1 year and evaluation was done.
The effects of change were improvement in mother’s knowledge
with score of > 75% from 11.1% to 79.6%, improvement in
knowledge among health staff with > 75% score from 12.1% to
81.8%. Indicator achieved 77.1% as compared to 98% target set.
- OUTLINE
OF PROBLEM
Childhood
immunization is the most effective method of preventing infectious
diseases. With the successful implementation of the national
immunization programme over the 20th century, it has
seen a tremendous reduction in mortality and morbidity of
immunisable diseases.
Unfortunately
the benefit of immunization may be the score of immunization side
effects as seen in Australia in 1970-80. Due to overconcern of
parents on the side-effects of some immunization, the immunization
coverage have fallen below the level that confers herd immunity.
It has caused an outbreak of pertussis. Effective immunization has
resulted in eradication of some diseases in the world such as
smallpox and polio.
Immunogenicity
survey with DPT booster by T.Nolan et al (1998) among 100 toddlers
attending MCH clinic Melbourne noted raised Ab level to
immunization after 4 – 6 weeks of DPT booster. Soong (1972) in
Semenyih noted that among the reasons for poor immunization
coverage among pre-schoolers were poor knowledge on importance of
immunization, schedule of immunization, perception to post-immunisation
side effects etc. The immunization coverage has been low among
toddlers in Pendang.
Table
1: DPT / polio booster coverage among toddler, 2000 – 2003 in
Pendang District
|
Health
facilities
|
2000
|
2001
|
2002
|
2003
|
|
KK
Pendang
|
69.4%
|
61.1%
|
54.3%
|
53.3%
|
|
KK Sungai
Tiang
|
61.9%
|
64.0%
|
70.5%
|
69.6%
|
|
KK Kubur
Panjang
|
53.7%
|
58.4%
|
65.0%
|
70.9%
|
|
Private
|
1.9%
|
0.9%
|
1.6%
|
0.0%
|
|
District
|
66.4%
|
62.0%
|
60.9%
|
59.3%
|
Table 2:
DPT and DPT Hib 3rd dose in Health Clinics in Pendang
District, 1999 – 2003
|
Health
facilities
|
1999
|
2000
|
2001
|
2002
|
2003
|
|
KK
Pendang
|
87.2%
|
95.7%
|
97.7%
|
91.7%
|
95.5%
|
|
KK Sungai
Tiang
|
73.9%
|
89.4%
|
99.5%
|
101%
|
111.9%
|
|
KK Kubur
Panjang
|
71.7%
|
77.1%
|
110.4%
|
103.5%
|
101.8%
|
|
Total
|
82.5%
|
93.3%
|
100.6%
|
99.9%
|
100.9%
|
- PROBLEM
IDENTIFICATION
The district
Quality committee meeting was conducted in November 2003 to
identify quality problems in the district. A brain storming
session were done involving 7 members. Some of the quality
problems identified were:
-
e-sample for Food Act and regulation contravention not
achieving 90% standard
-
poor coverage of premises during Aedes survey
-
inactive Dengue Free School programme
-
poor retrieving of chronic disease records
-
poor control of diabetics
-
poor control of hypertension
-
poor ABC delivery
-
poor coverage of booster immunization among toddlers
The
quality problems were prioritized by voting using the smart
criteria. After voting by the 7 members, the problem of poor
coverage of booster immunization among toddlers was chosen as the
DSA of the district.
- PROBLEM
ANALYSIS
Problem
analysis was done and 4 factors were identified as the
contributing factors namely:
- poor
toddler attendances
- poor
emphasis on toddler health services
- inaccurate
health education information
- poor
monitoring of achievement
- missed
opportunities not identified
KEY
MEASUREMENT FOR IMPROVEMENT
Indicator
chosen was booster dose immunization coverage among toddler and
the standard set was 95%.
Model of
good care:
|
Process
|
Criteria
|
Standard
|
|
1. Filing
system
|
- cards
are filed according to immunization status – complete or
incomplete
- appt
date given during clinic session
|
100%
100%
|
|
2.
Defaulter tracing
|
-
defaulter tracing in 1 wks
|
100%
|
|
3.
Monitoring of immunization achievement
|
- monthly
monitoring of immunization coverage
- setting
monthly achievement 7.92%
|
100%
90%
|
|
4. Missed
opportunities
|
- toddler
case referral from OPD to MCH
|
100%
|
|
5. Poor
knowledge of mothers on importance of toddler’s health
|
-
knowledge of mothers on toddlers health achieving > 75%
score
- monthly
health education to mothers
|
80%
100%
|
|
6.Toddlers
activities at clinic sessions achieving 3/3:
- health
talks
-
assessment on development
-assessment
on health
|
- toddler
activities according to schedule
|
100%
|
|
7.
Assessment and development of toddler
|
-
schedule growth development according to age
|
100%
|
|
8. health
education to staff
|
- toddler
health course
|
Once
a year
|
|
9.
Effective supervision at KD and KK
|
-
supervision monthly at KD and KK
|
One
a month
|
5.
PROCESS OF GATHERING DATA
5.1
General objective
To increase the
immunization coverage among toddler attending KK in Pendang
district from 60.9% to 95% by end of 2004
5.2
Specific objectives
5.2.1 To
ascertain reasons and factors contributing to poor boostser
immunization coverage among toddler in KK
5.2.2 To
ascertain knowledge of mother and staff on the importance of
toddler health care
5.2.3 To design
and implement remedial measures
5.2.4 To
reevaluate the remedial measures implemented
5.3
Methodology
5.3.1
Research methodology
A cross
sectional study for knowledge of mothers and staffs on booster
immunization and toddler health care.
5.3.2
Sampling method
Systematic
random sampling of 54 mothers for 3 clinics. These mothers have
toddlers who have incomplete booster immunization. 66 nursing
staffs were selected for the study.
5.3.3
Sample
The samples for
mothers were those with toddler age between 18 months and 4 years
and have defaulted for booster dose or defaulted clinic sessions.
5.3.4
Data collection
Questionnaires
for mothers were prepared and pre-tested before the survey.
Interviews with mothers were done by trained staff.
5.3.5
Definition
Toddler health
care – it includes health care given to toddler between 1.5 –
4 yrs old covering development assessment, health examination,
immunization booster, minor treatment, health education such as
health talks, cooking demonstration and defaulter tracing.
Toddler –
children between the age of 1.5 – 4yrs old
Defaulter to
booster immunization – Immunisation given after 1 yr of DPT 3rd
dose or DPT Hib and did not attend according to appointment date
given
Defaulter
tracing – Defaulter tracing within 1 week defaulting from
appointment date
Inclusion
criteria:
Toddler
residing in Pendang during study period
Exclusion
criteria
Those who
were not resident of Pendang and transfer in cases.
5.3.7
Data analysis
Data
analysis is done manually and Epi Info software
- ANALYSIS
AND INTEPRETATION
Study
done in February 2004 involving 54 mothers and the findings were:
5.1
88.8% of mothers were between the 20 – 39 yr old, 92.5%
were Malays, 44.4% were housewives, 63% had secondary school
qualifications and 51.9% had an income of RM501 – RM1000 /
month. 11.1% of mothers obtained a score of more than 75%.
5.2
12.1% of staff had a score of more than 75% score and the
majority (69.7%) had a score of 60 – 74% .
- STRATEGIES
FOR CHANGE
6.1
Remedial measures
- filing
of toddlers card
Toddler cards
are filled according to immunization completion
Appointment
dates are given to mothers during clinic sessions
- defaulter
tracing
To keep aside
toddlers cards that default clinic sessions at the end of the
sessions.
Toddlers
defaulting clinic sessions / immunization to be traced within 1
wk.
- Monitoring
of booster immunization during MCH meeting
Monthly
immunization monitoring during MCH meeting.
Monthly
immunization target set at 7.9% / month.
- Missed
opportunities
Given briefing
for MA and MO on immunization schedule and importance of
immunization
To get
immunization history for toddler attending OPD for treatment.
Referral of
missed opportunities to OPD and MCH
- Poor
knowledge on importance of toddler health done
KP study on
mothers with toddlers and staffs.
- Improve
on toddler activities at KK
Health
education talks
Cooking
demonstrations for toddlers
Cooking
demonstrations for mothers with toddlers
- Growth
assessment and development assessment of toddlers
Development
assessment according to schedule
Milestone
assessment.
- Health
education
Toddler health
care course.
KP study on
health care for health staff
- Supervision
during clinic sessions
Supervision
schedule for staff.
8.
EFFECTS OF CHANGE
|
Process
|
Criteria
|
Standard
|
Before
|
After
|
|
1. Filing
system
|
- Filed
according to immunization status
- Appointment
date given after clinic sessions
|
100%
100%
|
0%
60%
|
3866/4183
(92.4%)
3878/4183
(92.7%)
|
|
2.
Defaulter tracing
|
- Defaulter
tracing in 1 wk
|
100%
|
0%
|
843/925
(91.1%)
|
|
3.
monitoring of immunization coverage
|
- Monitoring
of immunization achievement
- Set
monthly target for KK and KD 7.92% ( for target of 95% /
year)
|
100%
90%
|
0%
0%
|
6/7
(85.7%)
16/20
(80.0%)
|
|
4. Missed
opportunities
|
- Referral
from OPD to MCH toddler with incomplete immunisation
|
100%
|
0%
|
2
(100%)
|
|
5.
Poor knowledge of mothers on importance of toddler health
care
|
- >
80% of mothers with knowledge score of > 75%
- Health
education on toddler health every month
|
80%
100%
|
11.1%
80%
|
79.6%
100%
|
|
6.
Activities for toddlers to achieve 3/3:
·
Talk on importance of booster immunisation
·
Development evaluation
·
Milestone
evaluation
|
- According
to schedule for toddlers
|
100%
|
33%
|
2035/2523
(80.6%)
|
|
7.Development
and milestone assessment
|
According
to schedule for toddlers
|
100%
|
70%
|
2035/2523
(80.6%)
|
|
8.
Improve knowledge of staff on health care for toddlers
|
- Course
for toddler health care
|
Once
a year
|
Not
done before
|
2
x
|
|
9.
Strengthen supervision
|
- supervision
per KD/ KK/mth
|
1
KK/KD month
|
70
(50%)
|
140
sessions
|
The
immunization coverage for booster has improved from 60.9%
to 77.7% by the end of 2005.
- THE
NEXT STEP
The benefits
obtained from this project are:
- Improvement
in booster immunization coverage
- Defaulter
tracing has improved
- Booster
immunization achievement is monitored monthly
- Improvement
in toddler health care – case filing, defaulter tracing,
assessment according to schedule, activities for toddlers etc
- Improvement
in knowledge of mothers and staff on toddler health care and
booster immunization
As a follow-up
of this project, the management of toddler with malnutrition will
be looked into.
- REFERENCES
8.1 Annual
report for District of Pendang
8.2 Annual
report of Ministry of Health
8.3 Nolan T,
Altmann A, Hogg G, Skeljo M, Schuerman L, Antibody persistence,
PRP – specific immune memory and booster responses to DTPa/Hib
vaccine in children with a new combination vaccine DTPa-HBV-IPV/Hib
at 2,4, and 6 months of age, University of Australia, Vaccine
Research Conference, 2001
8.4 Soong,F.S,
1971/72, The immunization status of some preschool children in a
new village in West Malaysia, Medical Journal of Malaysia, Vol,26,
page 90-93
***************************************************************************
To
reduce the waiting time of patients with chronic diseases
at
Pendang HC and Kubur Panjang HC at Pendang District, Kedah, 2002
1.
OUTLINE OF PROBLEM
Client’s
satisfaction is defined as feeling satisfied, safe and trusting
the services given to client. Satisfaction is achieved when the
product or services given achieves or satisfies the
wants/specification and perception of clients. It is important as
it influences the health seeking behaviour of clients, compliance
to treatment and fostering good relationship with provider. This
component encompasses a satisfied way of life when a person
achieves better quality of life (Larsen et al, 1976). Waiting time
is one of the components of patient satisfaction and this will
influence the patients’ compliance to follow-up and treatment.
Both components are crucial in ascertaining the quality of
services, care and life of a patient with chronic illness.
Client
satisfaction survey has been conducted in all the HCs in Pendang
since 1997 and it has achieved 83% clients satisfied with the
services. A total of 2.7% were not satisfied with the services
given. Some 82.4% of clients felt that the services given was good
as compared to 8.1% clients felt it was unsatisfactory.
97.3% of respondent felt the staffs were helpful and
willing to help. A total of 78% felt the counter services were
good. 61.7% felt the facilities provided were satisfactory. (Zainal
Che Mee et al, 1997).
A
brain mapping session was conducted with the head of units to
identify the quality problems in each unit and the committee came
up with 7 main quality problems. The nominal group technique was
used to prioritise the quality problems identified by using the
SMART criteria. Voting was done on the quality problems identified
earlier namely high perinatal mortaliry rate, long waiting time at
Pendang HC and Kubur Panjang HC and moderate and severe anaemia
among mothers at 36 weeks of gestation.
Long waiting
time was chosen as quality problem that require urgent action and
remedial measures. The other two issues are addressed in perinatal
mortality audits and safemotherhood initiative project
respectively.
Clients
are influenced by many factors such as individual influencers
namely information processing, believe, learning behaviour,
motivation and behaviour, persuasive communication and decision-
making (Mowen, 1990). Clients are also influenced by environmental
factors such as situation, group, family, culture, subculture,
economic or policy/regulation about health services.
Parasuranam
et al (1990) found that 4 main factors that influence client
satisfaction such as word-of-mouth communication, personal needs,
previous experience and external communication.
A
study done by A. Shukur A. Hamid (1993) in Hospital Kangar noted
that the waiting time to see a Dr. is between 29.7 min – 35.5
min. The study in Kuala Krai, Kelantan noted that the waiting time
to see Dr was between 3 min to 1 hr 45 min. The reasons for the
long waiting time were too many patients, inadequate staffing and
lost/unfound cards (Abraham, 1993).
Waiting
time has an influence on the attendance of patients as observed by
Lim (1991) in his study in Hospital Mentakab, Pahang among
hypertensive clinic defaulters. He noted that 72% of defaulters
gave reasons for defaulting as long waiting time. A verification
study was carried out at OPD Pendang HC in July 2001 and noted the
waiting time for chronic patients to be:
Registration
30 min
Waiting to see Dr
60 min
Treatment
by Dr/MA 10 min
Laboratory
12 min
Pharmacy
20 min
Total
time
132 min
The
waiting time for cold cases:
Registration
30 min
Waiting
to see Dr
15 min
Treatment
by Dr./MA 10 min
Pharmacy
10 min
Total
65 min
Pendang
Health Office has received 3 public complaints about the waiting
time for the first 6 months of 2001 in Pendang HC.
This
problem if not addressed, will cause much anxiety, erode the
confidence and morale of patients and affect the image of the
department.
Some
of the causes identified for the long waiting time were:
- Job description not
clear and specific among the unit in OPD
- No systematic triaging
and registration
- Patients do not follow
the appointment date given
Remedial
measures that will be implemented and will be an indicator of
improvement are:
- Waiting time as
according to the client’s charter
- No public complaints
from patients or relatives
- Improvement of the
clients’ satisfaction
A
problem analysis was done to identify the possible contributing
factors to the long waiting time. These factors were identified
as:
·
Delay in registration which may be attributed to
non-compliance to appointment, cards not filed according to
appointment date, inadequate staffing, losing follow-up card and
patient’s attitude
·
Delay in treatment which may be attributed to no
screening/triaging, inappropriate referral and too many referral
by MAs to MO.
·
Delay in laboratory investigation such as inadequate
staff, inappropriate lab test and attitude of staff.
·
Delay in dispensing medication may be attributed to
countersigning of List A drugs, poor legibility of prescription
slips and attitude of staff and patients.
- KEY
MEASUREMENTS FOR IMPROVEMENT
The
indicator selected to measure the performance of remedial measures
taken is the percentage of patients with chronic diseases waiting
more than 90 min from registration
to obtaining medication from pharmacy.
The
standard set is not more than 50%.
Model
of good care was formulated according to the process, criteria and
standard set. The processes that were identified as critical
process and if control will eventually affect the overall
indicator and standard set were:
- Registration time
- Clinical examination
- Laboratory examination
- Health education
- Filing system
- Dispensing of medicine
Table
1: Model of good care
|
process
|
criteria
|
Std
|
Performance
Before
remedial measures
|
|
Registration
|
<
15 min
|
100%
|
PHC
57.2%
KPHC
40%
|
|
Clinical
exam
|
Screening
for BP and BW
|
100%
|
PHC
80%
KPHC
100%
|
|
Lab
exam
|
<
15 min
|
100%
|
PHC
78%
KPHC
65%
|
|
Filing
system
|
Card
retrieve a day before clinic session
|
100%
|
PHC
70%
KPHC
60%
|
|
Dispensing
of medication
|
Medication
given are adequate
|
100%
|
PHC
90%
KPHC
70%
|
- PROCESS
OF GATHERING OF INFORMATION
A
few studies have been planned to gather information about the
system at HC.
3.1
The objective of the study is to reduce the waiting time
from 2 hr to 90 min for patients with chronic disease at Pendang
HC and Kubur Panjang HC
The
specific objectives were to:
3.2
To identify contributing factors to the long waiting time
3.3
To identify which section contribute to the long waiting
time from
bregistration to treatment
3.4
To plan the remedial and implement measures
3.5
To perform evaluation study on the remedial measures
instituted
Methodology
for collection of information includes the following:
- Time motion study
- Observation at laboratory and
registration
- Study of prescriptions at
pharmacy
- Study on appropriate referral
to MOs
The
study includes all patients with chronic diseases getting
treatment from Pendang HC and K,Panjang HC excluding cold cases
and emergency cases seen after office hrs.
The
information gathered were analysed manually and analysed by Epi
Info version.
- ANALYSIS AND
INTERPRETATIONS
4.1
Time motion study
From
the time motion study done in both Pendang HC and K.Panjang HC
noted that the waiting time was 174 min and 97.9 min respectively.
Table
2: Time motion study findings at Pendang HC and K.Panjang HC
|
Process
|
Pendang
HC
|
K.Panjang
HC
|
|
Registration
|
47
min
|
22.5
min
|
|
Waiting
for treatment
|
49
min
|
23.6
min
|
|
Treatment
for Dr MA
|
22
min
|
12.8
min
|
|
Laboratory
|
29
min
|
17
min
|
|
pharmacy
|
12
min
|
22
min
|
4.2
Observation of filing system and registration
4.2.1
Findings of filing system
- Card filing done
according to identity card number
- Chronic pt cards not
filed separately because of space constraints
- Cards were retrieved a
day before clinic sessions
- Only 57.2% got their
queue number by 15 minutes in Pendang HC as compared to 60% in
K.Panjang HC.
4.3
Clinical examination / screening
- 80% were examined for BP
and weight in Pendang HC as compared to 100% in K.Panjang HC
before seeing M&Hos or MAs
4.4
Laboratory examination
- 78% patients got
laboratory results (FBS / HbA1c) by 15 min in Pendang HC and
65% in K.Panjang HC
4.5
Pharmacy
- Only 70% patients said
that the medication given was enough for the next follow-up in
Pendang HC and 90% in K.Panjang HC
4.6
Cases seen by M&HO
M&HOs
were seeing 77.6% of uncomplicated hypertensives and 75.3%
uncomplicated diabetics. This will increase the waiting time to
see M&HOs because they are seeing cases that can be managed by
MAs.
4.7
Prescriptions at pharmacy
Incomplete
prescriptions were not a problem at Pendang HC (<3%) but it
increased during special clinic sessions. Prescriptions that were
required to be countersigned by FMS were only < 10% of the
total prescriptions.
- STRATEGY FOR CHANGE
Several
strategies for change or remedial measures were planned and
implemented.
5.1
Colour coding of chronic cases according to criteria. The
cards of patients were tagged according to colours such as green,
white and red. Green tag are stable cases and can be managed by
MA. White tags are cases with one abnormal criteria and red tags
are cases with more than one abnormal criteria. The criteria
included are body weight, BP, urine sugar, FBS, HbA1c, urine
albumin, frequency of asthmatic attack, peak flow chart etc. These
criteria are based on the CPG produced by Ministry of Health.
These cases will be reviewed by M&HO according to specified
intervals.
5.2
Filing system
The
chronic diseases card were filed separately from the usual OPD
cases and the cards were retrieve one day before the clinic
sessions.
5.3
Staggering the patients by hour.
The
patients are staggered according to the hour. This will need the
patients’ full cooperation. They are required to put in their
appointment card according to the hour of appointment for the day.
5.4
Promoting the new work process
A
pamphlet was designed to inform patients their responsibility and
rationale of keeping to the appointment date given.
6.0
EFFECTS OF CHANGE
A
restudy was done in June 2002 after the remedial measures were
instituted for 3 months.
6.1
Time motion study
The
waiting time has reduced from 174 min to 59.9 min in Pendang HC
but increased from 97.9 min to 149.73 min in K.Panjang HC.
In
Pendang HC it was noted there was reduction in waiting time at
several processes such as registration, waiting to see M&HO/MA
and pharmacy. In K.Panjang HC there was increased waiting time in
almost all the processes except for waiting to see M&HO / MA,
laboratory and taking medication from pharmacy.
6.2
Clinical examination
100%
of patients in both the clinics were examined before seeing
M&HO or MA.
6.3
Laboratory examination
In Pendang
HC, only 40% of patients obtain their laboratory results by 15 min
whilst 37.9% of patients in K.Panjang receive their results by 15
min.
6.4
Health education sessions
All
patients at both clinics were provided with pamphlets concerning
the new work process.
6.5
Medications
Only
85.9% of patients in Pendang HC had adequate supply of medications
as compared to 62.1% of patients in K.Panjang HC.
It
was noted that patients waiting more than 90 min in Pendang HC
were 87.1% (83) and in K.Panjang HC was 82.8% (24) waited more
than 90 min.
It
was noted that lack of staff affected the achievement of this
indicator and standard. The situation in Pendang HC and K.Panjang
HC differ in staff strength and facilities available such as HbA1c
and microalbumin which is available only in Pendang HC. These two
test took an average of 20 min to perform. This will greatly
affect the waiting time. There are 3 Mas and 2 M&HO in Pendang
HC as compared to one M&HO and 2 Mas in K.Panjang HC.
The
tangible benefit that was obtained in this study was the waiting
time has reduced tremendously and achieved 87.1% in Pendang HC.
There were no complaints of long waiting time for the last 3
months of implementation. The consultation time with Dr. was used
to use for clinical management of the case. There was defined work
process and job division between staffs. Innovation on colour
coding was able to reduce the inappropriate cases seen by Dr.
Special
thanks to:
Dr.Hayati
Mohd. Radzi, Dr.Baizury Bashah, Dr.Hazik Jamil Khan, Dr.Loh Leh
Teng, Ishah Rashid, Faisol Abdul Rahim, Hussein Abdul Rahim,
Zainol Man.
ABSTRACT
To reduce the waiting time of patients
with chronic diseases at Pendang HC and Kubur Panjang HC at
Pendang District, Kedah, 2002
Dr.Hayati
Mohd. Radzi, Dr.Baizury Bashah, Dr.Hazik Jamil Khan, Dr.Loh Leh
Teng, Ishah Rashid, Faisol Abdul Rahim, Hussein Abdul Rahim,
Zainol Man.
Long
waiting time has been one of the components of client’s
satisfaction. It is important as it influences the health seeking
behaviour of clients, compliance to treatment and fostering good
relationship with provider. Client satisfaction survey has been
conducted in all the HCs in Pendang since 1997 and it has achieved
83% clients satisfied with the services.
The
indicator selected to measure the performance of remedial measures
taken is the percentage of patients with chronic diseases waiting
more than 90 min from registration
to obtaining medication from pharmacy. Model of good care was
formulated with certain process, criteria and standard. The
remedial measures taken were colour coding for cards, filing
system, retrieval of cards, appropriate referral for Dr. and
promotion on keeping to appointment date. After implementation of
the remedial measures, the waiting time improved for Pendang HC by
87.1% of clients waited less than 90 min but 82.2% of clients in
K.Panjang HC waited more than 90 min.
*************************************************************************
SAFE
MOTHERHOOD INITIATIVE DAERAH PENDANG
Hayati
Md. Radzi, Baizury Bashah, Ishah Rashid, Maimunah Md Noor, Azizah
Ramli, Saliha Hashim, Che Olah Zakaria
TAJUK:
Meningkatkan pengamalan perancang
keluarga di kalangan ibu berisiko tinggi di daerah Pendang dari
45.8% ke 80 % menjelang
tahun akhir tahun 2004
1.0
PENDAHULUAN LATAR
BELAKANG
Daerah
Pendang dengan keluasan 626.14
km persegi dengan jumlah penduduk sejumlah 97,850 yang
terdiri dari 80%
Melayu, 7.9 % Cina , 7.7 % Siam dan 1.4 % India dan lain-lain
bangsa. Pekerjaan utama penduduk di daerah Pendang adalah dalam
sektor pertanian, penoreh, pesawah, berniaga, pekerja kilang,
peniaga dan kakitangan kerajaan.
Fasiliti
kesihatan di daerah Pendang adalah terdiri dari 3 buah klinik
Kesihatan serta 17 buah Klinik Desa yang memberi kemudahan
kesihatan kepada masyarakat di daerah ini. Hospital terdekat iaitu
Hospital Alor Star adalah terletak 30 km dari Pendang.
Perkhidmatan
kesihatan mudah diperolehi dengan terdapatnya kemudahan jalanraya
yang menghubungi hampir
90% kampong-kampong
di daerah ini. Rata-rata di kawasan pendalaman masyarakat
menggunakan kenderaan bermotor sebagai pengangkutan untuk
perhubungan. Bekalan air dan tandas mencapai hampir 100%.
Masalah
kesihatan yang dikenalpasti di daerah Pendang
bagi bahagian Kesihatan Ibu dan anak ialah seperti
masalah anaemia yang masih di pantau dalam Projek SMI tahun 2002 dan adalah berterusan, masalah kedua adalah
liputan imunisasi booster rendah di kalangan toddler dan ini telah
di buat kajian DSA bagi tahun 2004.
Masalah
kekurangan amalan perancang keluarga di kalangan ibu berisiko
adalah masalah yang juga di kenalpasti dan telah di pilih sebagai
projek Safe motherhood Initiative bagi daerah Pendang bagi tahun
2004.
2.
PENYATAAN MASALAH
2.1
PEMILIHAN MASALAH
JK
Kualiti telah bermesyuarat pada bulan Oktober 2003 dan
menyenaraikan beberapa masalah kualiti bagi semua unit. Antara
masalah yang dikenalpasti untuk Program Pembangunan Keluarga.
Pemilihan masalah ini dilakukan dengan menggunakan Kaedah
“Nominal Group Technique”.
Antara
masalah Kualiti yang dikenalpasti ialah:
2.2.1
Kurang kelahiran di ABC di ketiga-tiga Klinik Kesihatan
2.2.2
Kadar kematian perinatal yang tinggi di daerah Pendang
2.2.3
Keciciran yang tinggi di kalangan toddler
2.2.4
Liputan pelalian di kalangan toddler yang tidak mencapai sasaran
98%
2.2.5
Liputan pap smear yang tidak mencapai sasaran 2,300 yang
ditetapkan
2.2.6
Kadar unsatisfactory pap smear yang tinggi iaitu > 5%
2.2
MENGUTAMAKAN MASALAH
Ahli
mesyuarat telah menjalankan pengundian mengikut kriteria SMART dan
masalah yang
mencapai markah tertinggi dipilih untuk projek safe
motherhood initiative ini.
Berdasarkan
kepada kajian dan analisa kes-kes ibu berisiko yang telah bersalin
tahun 2002 terdapat penurunan sehingga 2.3% pengamalan sejak tahun
2001 adalah 72.4%. Paling ketara di KK K. Panjang perbezaan adalah
sehingga 4.4 %. Sasaran yang di tetapkan bagi daerah Pendang ialah
80%, manakala pencapaian daerah bagi tahun 2001
ialah
75.7% dan 72.4 % pada tahun 2002 seperti dalam
carta 1:
 Pencapaian prestasi
pengamalan P/Keluarga di
kalangan IHBT di Daerah Pendang dari Januari hingga Oktober 2003
ialah 45.8% sahaja dan dianggarkan pencapaian pada tahun 2003
ialah 54.96%. Ini menunjukkan sasaran tidak tercapai sebanyak
25.1% berbanding dengan sasaran yang telah ditetapkan iaitu 80%.
Pencapaian prestasi
pengamalan P/Keluarga di
kalangan IHBT di Daerah Pendang dari Januari hingga Oktober 2003
ialah 45.8% sahaja dan dianggarkan pencapaian pada tahun 2003
ialah 54.96%. Ini menunjukkan sasaran tidak tercapai sebanyak
25.1% berbanding dengan sasaran yang telah ditetapkan iaitu 80%.
Jadual
1: Jumlah kes Ibu Berisiko yang
mengamal perancang keluarga mengikut Kelinik Kesihatan tahun 2001
–2002
|
KEMUDAHAN
KESIHATAN
|
JUMLAH
KES BERISIKO TINGGI
|
PERATUS
KES BERISIKO YG MENGAMAL P/KELUARGA
|
|
2001
|
2002
|
2001
|
2002
|
|
KK
PENDANG
|
15.6
(173/1112)
|
12.0
(116/965)
|
75.5
(131/173)
|
74.1
86/116
|
|
KK
SG. TIANG
|
29.4
118/402
|
29.8
108/363
|
72.0
85/118
|
70.4
76/108
|
|
KK
K. PANJANG
|
24.2
88/364
|
22.5
73/325
|
77.3
68/88
|
72.6
53/73
|
|
DAERAH
|
19.96
375/1878
|
17.96
297/1653
|
75.7
284/375
|
72.4
215/297
|
Perkhidmatan
penjagaan ibu bermula
dari semasa mengandung, semasa proses kelahiran dan
ketika postnatal selama 42 hari. Ibu mengandung yang
dikenalpasti mempunyai masalah obstetrik semasa, perubatan atau
mempunyai sejarah masalah obstetrik yang lalu akan dikodkan
berisiko tinggi berdasarkan senarai semak yang dikenalpasti.
Senarai semak faktor risiko ini meliputi penjagaan semasa tempoh
antenatal, intrapartum dan postpartum. Ibu hamil berisiko tinggi
ditakrifkan ibu yang diberikan tag bewarna kuning dan merah sahaja.
Jadual
3: Kadar kematian ibu daerah Pendang bagi 2001 –20002
|
KEMUDAHAN
KESIHATAN
|
KADAR
MATERNAL MORTALITI
|
|
2001
|
2002
|
|
|
KK
Pendang
|
0.94
(1)
|
18.7(2)
|
|
|
KK
Sg. Tiang
|
2.56
(1)
|
0
|
|
|
KK
K.Panjang
|
0
|
0
|
|
|
DAERAH
|
11.1
/10000
|
17.1/10000
|
|
2.3
MAGNITUD MASALAH
Penurunan
ketara dikesan berlaku di KK K. Panjang iaitu 4.3%. Daerah Pendang
menunjukkan penurunan peratus pengamalan perancang keluarga
sebanyak 3.3%. (Sila rujuk Jadual 1)
Jadual
4: Jadual frekuensi kematian dan amalan perancang keluarga di
kalangan IBT di daerah Pendang, 2002
|
KES
|
2001
|
2002
|
|
Antenatal
Baru
|
1878
|
1653
|
|
Ibu
Hamil Berisiko Tinggi
|
375
(19.96%)
|
284
(17.96%)
|
|
Ibu
berisiko mengamal P/Keluarga
|
284
( 75.7%)
|
215(72.4%)
|
|
Ibu
berisiko tidak mengamal P/Keluarga
|
91
(24.3%)
|
82
( 27.6%)
|
|
Ibu
tagging merah yang mengamal P/Keluarga
|
49
(13.1%)
|
27
(9.9%)
|
|
Ibu
taging kuning yang mengamal P/Keluarga
|
235
(86.9%)
|
257
(90.5%)
|
|
Kematian
Perinatal dikalangan ibu IBT yang tidak mengamal
|
0
|
0
|
|
Ibu
PIH yang tidak mengamal P/Keluarga
|
156
(41.6%)
|
112(39.4%)
|
|
Kematian
Ibu
|
0
|
1
(100% )
|
|
Kematian
ibu di kalangan ibu berisiko yang tidak mengamal P/Keluarga
|
0
|
0
|
2.4
KESAN MASALAH
Dengan
projek safe motherhood ini adalah diharapkan, daerah akan dapat
meningkatkan amalan perancang keluarga di kalangan ibu berisiko
tinggi dan dapat mengurangkan masalah yang berlaku berikutan dari
masalah IBT. IBHT meningkatkan morbiditi dan mortaliti ibu dan
bayi. Dengan mengamalkan perancang keluarga yang berkesan,
morbiditi dan mortaliti akan dapat dikurangkan. Dengan menjalankan
tindakan penambahbaikan / pemulihan adalah diharapkan peratus
pengamalan perancang keluarga akan meningkat bagi daerah Pendang.
3.0
METODOLOGI
3.1
Jenis kajian
Satu
kajian retrospektif telah dijalankan pada bulan November 2003
melibatkan ketiga-tiga Klinik Kesihatan di daerah Pendang.
3.2
Kaedah sampling dan unit sampel
Sampel
yang dipilih ialah ibu postnatal yang berisiko yang bersalin dari
Januari – Disember 2002 di ketiga-tiga Klinik Kesihatan.
Systematic random sampling telah dilakukan untuk pemilihan sampel.
Sejumlah 108 ibu postnatal yang berisiko telah dipilih untuk
kajian awal ini.
3.3
Metodologi kajian
Kajian
dilakukan menggunakan borang soalselidik yang telah direka dan
dilakukan pretest di kalangan ibu mengandung. Pengubahsuaian
dilakukan mengikut maklumbalas dari pretest. Kajian dilakukan oleh
JK dan JD yang telah diberikan taklimat mengenai pengisian borang
soalselidik. Ibu postnatal yang berisiko tinggi yang terpilih
dibuat lawatan ke rumah untuk kajian mengenai temubual.
3.4
Kriteria inklusi
Semua
ibu postnatal berisiko tinggi yang didaftarkan di daerah Pendang
dan berada di daerah semasa tempoh kajian dilakukan.
3.5
Kriteria eksklusi
Ibu
yang telah berpindah atau tiada dalam kawasan semasa kajian
dilakukan.
3.6
Definasi
3.6.1
Mengamalkan perancang keluarga
Ibu
postnatal yang mengamalkan kaedah perancang keluarga yang berkesan
iaitu meliputi kaedah-kaedah pil, kondom, IUCD, norplant,
injection, BTL, vasektomi dan lain-lain kaedah.
3.6.2
keciciran perancang keluarga
Ibu
yang gagal datang ke klinik untuk perkhidmatan perancang keluarga
mengikut tarikh temujanji yang diberikan.
3.6.3
Pengesanan keciciran perancang keluarga
Setiap
kes yang tercicir perlu dikesan dalam 48 jam selepas sessi klinik
samada melalui lawatan ke rumah, surat atau telefon.
3.6.4
Kesan sampingan perancang keluarga
Kesan
sampingan seperti loya, muntah, pening, gemuk, break through
bleeding, irregular bleeding, amenorrhoea, dan lain-lain. Kesan
sampingan ini akan berhenti / hilang apabila ibu berhenti
menggunakan kaedah tersebut.
3.6.5
ibu berisiko tinggi
Ibu
postnatal yang dikesan berisiko semasa mengandung dan ditagkan
dengan kod bewarna kuning dan merah.
3.6.6
Ibu merisiko tinggi
Ibu
yang menerima salah satu kaedah perancang keluarga
sekurang-kurangnya selama 6 bulan.
4.0
ANALISA MASALAH
Sessi
percambahan fikiran telah dijalankan dan beberapa masalah yang
dikenalpasti yang menyumbang kepada kurang amalan perancang
keluarga (PK) di kalangan IBT.
Kurang
pengetahuan anggota dalam pengendalian perancang keluarga di
kalangan IBT mungkin disebabkan oleh kurang latihan mengenai
pengendalian PK di kalangan IBT, kurang penyeliaan anggota semasa
mengendalikan sessi perancang keluarga, kurang pendedahan kepada
kaedah PK yang sediada dan sikap anggota dalam mengendalikan kes
IBT.
Kelemahan
dalam pengendalian PK bagi IBT mungkin disebabkan oleh kurang
pengetahuan mengenai pengendalian PK, tiada pengesanan kes
tercicir dan tiada pengesanan kes IBT disebabkan oleh kurang
penyeliaan dan semakan senarai semak.
Kurang
pilihan kaedah perancang keluarga kerana pilihan kaedah yang
terhad, kurang promosi tentang kaedah PK dan kurang pengetahuan
mengenai kaedah yang dipilih.
Ibu
kurang komplians dalam mengambil kaedah PK kerana kurang
pengetahuan ibu/suami mengenai kaedah PK, suami tidak izinkan,
kesan sampingan PK dan pendidikan kesihatan yang kurang berkesan
serta sikap ibu. Sikap ibu mengenai amalan PK dipengaruhi oleh
budaya/kepercayaan persepsi mengenai PK dan pengalaman buruk yang
lalu.
5.
OBJEKTIF
5.1
OBJEKTIF UMUM
Untuk
memastikan amalan perancang keluarga di kalangan ibu berisiko
tinggi dari 45.8% ke 80% menjelang akhir tahun 2004 di daerah
Pendang.
5.2
OBJEKTIF KHUSUS
5.2.1
Untuk mengenalpasti sebab-sebab kurang amalan perancang keluarga
di kalangan ibu berisiko tinggi.
5.2.2
Menyediakan pelan tindakan dan langkah pemulihan.
5.2.3
Membuat penilaian berkala ke atas pencapaian indikator.
6.0
HASIL KAJIAN
Kajian
awal telah dijalankan di kalangan ibu berisiko tinggi (IBT)di
ketiga-tiga Klinik Kesihatan. Jumlah responden ialah 108 orang IBT
telah ditemuduga untuk bagi ibu yang telah bersalin dari Januari
– Disember 2002. Kajian telah dijalankan pada November 2003.
6.1
Hasil kajian
|
PARAMETER
|
FREKUENSI
(N=108)
|
PERATUS
|
|
1.
Kumpulan umur
<
20 tahun
20
– 34 tahun
35
– 40 tahun
>
40 tahun
|
0
77
27
4
|
0
71.3
25.0
3.7
|
|
2.
Kumpulan etnik
Melayu
India
Siam
|
104
1
3
|
97.2
0.9
1.9
|
|
3.
Status pendidikan
Tidak
bersekolah
Sek.
Ren.
Sek.
Men.
IPT
|
0
12
93
3
|
0
11.1
85.1
2.8
|
|
PARAMETER
|
FREKUENSI (N=108)
|
PERATUS
|
|
4.
Parity
Para
1
Para
2-5
>
para 5
|
14
75
19
|
12.9
69.4
17.5
|
|
5.
Pekerjaan
Suri
rumahtangga
Pekerja
kilang
guru
|
89
4
10
|
82.4
3.7
9.3
|
|
6.
Pendapatan
<
RM 500
RM501
– 1500
RM1501
– 2500
>
RM 2500
|
24
33
50
1
|
22.2
33.0
46.3
0.1
|
|
7.
Amalan perancang keluarga yang lalu
Pernah
amal
Tidak
pernah amal
|
59
49
|
54.6
45.4
|
|
8.
Kaedah PK
Tradisional
Pil
Kondom
Suntikan
Safe period/azal
|
9
55
28
4
12
|
8.3
50.9
25.9
3.7
35.2
|
|
9.
Sebab menggunakan kaedah tersebut
Mudah
Selamat
Menjarak
kelahiran
Tiada
respond
|
59
6
12
23
|
54.6
5.6
11.1
22.3
|
|
10.
Amalan PK sekarang
Pil
IUCD
Condom
Traditional
Injection
|
64
11
2
11
31
|
54.2
2.8
1.9
10.1
28.7
|
|
11.
Penggalak untuk mengamalkan PK
Suami
Sendiri
Staff
kesihatan
|
31
15
62
|
28.7
13.8
57.5
|
|
12.
Persepsi suami terhadap PK
Tidak
setuju
Tidak
yakin
setuju
|
6
2
100
|
5.6
1.9
92.6
|
|
PARAMETER
|
FREKUENSI
(N=108)
|
PERATUS
|
|
13.
Pilihan kaedah PK
Pil
Suntikan
BTL
IUCD
Tradisional
Tidak
jawab
|
46
33
6
30
11
28
|
37.0
30.5
5.5
28
10.1
25.9
|
|
14.
Tag
Merah
Kuning
|
22
86
|
20.4
79.6
|
|
15.
Faktor risiko
PIH
Anemia
Diabetes
Asthma
LSCS
Retained
placenta
|
46
18
13
10
13
8
|
42.6
16.7
12.0
9.3
12.0
7.4
|
|
16.
Pengalaman lalu
Pening
Loya
Haid
sedikit
Haid
Tak Tentu
Kegemukan
Terlupa
makan ubat
Tidak
datang Haid
Mengandung
ADR in situ
Tiada
masalah
|
17
17
8
8
7
3
1
1
46
|
|
|
17.
Kaedah-kaedah yang anda tahu?
5
kaedah
4
kaedah
3
kaedah
Tidak
jawab
|
40
6
3
59
|
37.0
5.5
2.8
54.6
|
|
18.
Sumber maklumat mengenai
kaedah
Majalah
Jururawat
Kawan
|
25
53
30
|
23.1
49.1
27.8
|
|
19.
Di mana PK diperolehi?
KK/KD
Farmasi/Kedai
ubat
|
92
16
|
72.2
27.8
|
|
PARAMETER
|
FREKUENSI
(N=108)
|
PERATUS
|
|
20.
Jika tak amal PK, kenapa?
Suami
tak izin
Air
susu kering
Lemah
badan
Mandol
Berat
badan bertambah
Sakit
kepala
Muntah
|
5
3
2
1
17
8
5
|
|
|
21.
Jika tidak amal apa berlaku?
Mengandung
Tidak
jawab
|
105
3
|
97.4
2.6
|
|
22.
Cara amalkan untuk jarakkan kandungan
Pil
Safe
period
IUCD
BTL
Suntikan
tradisional
|
54
10
8
5
12
14
|
50.0
9.3
7.4
4.6
11.1
13.0
|
|
23.
Keburukan kaedah moden PK
Tiada
Kering
air susu
Haid
tidak teratur
Pening
Gemuk
Mudah
terlupa makan pil
|
46
10
5
16
28
3
|
|
6.2 Pengetahuan ibu mengenai kaedah
perancang keluarga
|
Skor pengetahuan
|
Bilangan
|
Peratus
|
|
<
60%
|
28
|
25.9%
|
|
60
– 80%
|
72
|
66.7%
|
|
>
80%
|
8
|
7.4
%
|
ANALISA MASALAH KURANG AMALAN PERANCANG
KELUARGA
DI
KALANGAN IBU BERISIKO TINGGI DI DAERAH PENDANG

7.0 JADUAL INDIKATOR
PENILAIAN PENCAPAIAN SMI 2004 DAERAH PENDANG
1.HEALTH
INDICATOR
|
INDIKATOR
|
DEFINASI
|
SUMBER
|
DATA
ASAS
|
SASARAN
|
PENCAPAIAN
|
|
1.
% Pengamalan PK di kalangan IBT
|
Bil
IBT yang mengamal PK
X 100
|
Kad
KIK 1(b)96
KIB
101
|
45.8%
|
80%
|
bulanan
|
|
2.
Kadar kematian ibu IBT yang tidak mengamalkan PK
|
Bilangan
Kematian ibu IBT yg tidak amal PK
X 1000
Bilangan
IBT
|
Kad
KIK (b)/96
KIB
104
|
3.6/1000
|
0/1000
|
bulanan
|
8.0
KAEDAH PERLAKSANAAN LANGKAH PEMULIHAN
|
ISU
|
STRATEGI
|
AKTIVITI
|
TANGGUNGJAWAB
|
SASARAN
|
MASA
|
INDIKATOR
|
|
1.
Kurang pengetahuan dalam pengendalian PK untuk IBT
|
Meningkatkan
pengetahuan ibu melalui kaedah pendidikan kesihatan dan
penyeliaan berkesan
|
- Kursus /
latihan dalam perkhidmatan
-
Pengendalian PK
-
kemahiran IUCD
insertion
- Clinical
Nursing education
-
case study
- Penyeliaan
berkesan semasa sessi PK
-
laporan penyeliaan
mengikut format penyeliaan
- Kajian
mengenai pengetahuan IBT mengenai PK
|
PKD
KJK
JKU
KJK
JKU
|
anggota
kejururawatan
PP&K
|
Mac
2004
|
Bil.
kursus mengenai PK (2)
Bil
case study mengenai PK(1)
Bil
Penyeliaan mengikut format(45)
|
|
2.Kelemahan
pengendalian PK kpd IBT
|
Meningkatkan
pengendalian kes dan keciciran secara berkesan melalui
pengesanan keciciran dalam masa 48 jam
|
- Mengenalpasti
kes keciciran selepas sessi klinik
- Menjalankan
pengesanan keciciran melalui telefon atau lawatan ke
rumah
- Kaunseling
kepada ibu dan keluarga
- Semakan
kad PK semasa penyeliaan
|
JK/JD/BT
JK/JD
|
kes
keciciran
|
Januari
2004
|
bil
kes tercicir
(8.8%)
bil
pengesanan dalam masa 1 minggu
(
85 %)
bil
sessi kaunseling untuk kes tercicir (79)
semakan
kad semasa penyeliaan
|
|
ISU
|
STRATEGI
|
AKTIVITI
|
TANGGUNGJAWAB
|
SASARAN
|
MASA
|
INDIKATOR
|
|
3.
Kurang pilihan kaedah PK
|
Memastikan
pilihan kaedah PK yang mencukupi
|
- Memastikan
anggaran peruntukan dilakukan pada awal tahun
- Pesanan
dilakukan untuk bekalan yang mencukupi bagi 1 tahun
- Semakan
stok pada setiap bulan
- Pendidikan
kesihatan mengenai kaedah PK yang sediada kepada IBT
-
Ceramah
-
focus group
discussion (79)
|
KJK
JKU
|
anggota
kejururawatan
|
anggota
kejururawatan
IBT
dan suami
|
stok
bekalan mencukupi untuk 2 bulan
|
|
4.
Ibu tidak komplians kepada kaedah PK
|
Meningkatkan
komplians ibu kpd PK melalui pendidikan kesihatan berkesan
dan kaunseling serta membetulkan kepercayaan dan
mispersepsi mengenai PK
|
- Promosi
kesihatan yang berkesan kepada IBT
-
ceramah kesihatan
pada 36 minggu untuk IBT
-
kaunseling semasa
postnatal
-
FGD kepada ibu dan
suami
-
pamphlet kepada ibu
semasa sessi ceramah
- Kajian
mengenai pengetahuan anggota mengenai aspek PK dan
pengendalian kes PK
|
KJK
PP&K
JK
JD
BT
PJ
PP
JK
JD
|
IBT
|
IBT
dan suami
anggota
kejururawatan
|
IBT
diberikan ceramah kesihatan pada 36 minggu (208)
ibu
membuat pilihan kaedah PK pada 36 minggu
(579)
|
9.0
GANTT CHART UNTUK PERLAKSANAAN TINDAKAN PEMULIHAN /
PENAMBAHBAIKAN
|
AKTIVITI
|
JAN
|
FEB
|
MAC
|
APR
|
MAY
|
JUN
|
JUL
|
AUG
|
SEP
|
OCT
|
NOV
|
DIS
|
- Kursus/latihan
dalam perkhidmatan
-
pengendalian PK
-
kemahiran memasukkan
IUCD
|
|
|
x
x
|
|
|
|
|
|
|
|
|
|
|
2. Clinical nursing education
|
x
|
|
x
|
|
x
|
|
x
|
|
x
|
|
x
|
|
- Penyeliaan
berkesan
- laporan penyeliaan
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
|
4. Kajian
pengetahuan IBT mengenai PK
|
|
|
x
|
|
|
|
|
|
|
|
|
|
|
5. Pengesanan
keciciran melalui telefon atau lawatan ke rumah
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
|
6. kaunseling kepada ibu dan keluarga
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
|
7. Penyeliaan semasa sesi klinik PK
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
- Promosi
kesihatan kepada ibu dan suami (> 36 minggu dan
postnatal)
-
ceramah
-
FGD
-
kaunseling individu
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
- Bil
pamphlet diberikan kepada IBT semasa ceramah PK
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
x
|
- Kajian
mengenai pengetahuan anggota mengenai semua aspek PK
dan pengendalian kes PK
|
|
|
x
|
|
|
x
|
|
|
x
|
|
|
x
|
10.0
PENCAPAIAN INDIKATOR SMI
JANUARI – JUN 2004
1.HEALTH INDICATOR
|
INDIKATOR
|
DEFINASI
|
SUMBER
|
DATA ASAS
|
SASARAN
|
PENCAPAIAN
|
|
1. % Pengamalan PK di kalangan IBT
|
Bil IBT yang mengamal PK
X 100
|
Kad KIK 1(b)96
KIB 101
|
45.8%
|
80%
|
61.6%
(279/453)
|
|
2. Kadar kematian ibu IBT yang tidak mengamalkan PK
|
Bilangan Kematian ibu IBT yg tidak amal PK
X 1000
Bilangan IBT
|
Kad KIK (b)/96
KIB 104
|
3.6/1000
|
0/1000
|
0/1000
|
2.
SERVICE INDICATOR
|
INDIKATOR
|
DEFINASI
|
SUMBER
|
DATA ASAS
|
SASARAN
|
PENILAIAN
|
|
|
IBT yg diberi pen. kes pada 36 minggu
x 100
|
KIK 1(b)/96
|
34.7%
|
100%
|
69.1%
|
|
2. % IBT yang membuat pilihan mengenai kaedah PK
pada 36 minggu kandungan
|
IBT membuat pilihan kaedah PK
x 100
jumlah IBT pada 36 minggu
|
KIK 1(b)/96
|
NA
|
100%
|
57.3%
|
|
3. % ibu yang mempunyai pengetahuan yg mencukupi
(60%) mengenai PK
|
IBT yg mempunyai skor >60%
x 100
jumlah IBT yang terlibat dgn kajian
|
kajian irisan lintang
|
66.6%
|
75%
|
68.6%
|
|
4. % anggota kesihatan dengan pengetahuan > 80%
mengenai PK
|
Semua anggota kejururawatan yg mendapat skor >
80% mengenai perancang keluarga
x
100
|
pretest dan postest kursus PK
|
1.7%
(1/60)
|
75%
|
86.7%
(52/60)
|
|
5. % IBT yg tercicir dari klinik PK
|
Bil IHBT yang tercicir dari klinik PK X 100
Jumlah semua kes IBT yg mengamal PK
|
Kad KIK 1(b)/96
|
34.2
%
|
20
%
|
8.8%
|
|
6.% Keciciran akibat kesan sampingan kaedah PK
|
Bil penerima PK yang tercicir akibat tercicir akibat
kesan sampingan di kalangan IBT X 100
Jumlah penerima PK di kalangan IBT yang ada kesan
sampingan.
|
Kad PK
|
27.1%
|
15%
|
0%.
|
|
7. IBT yang mengamalkan PK sekurang-kurangnya 6
bulan selepas bersalin
|
Bil IBT yg amal PK sekurang-kurang 6 bulan selepas
bersalin x 100
Jumlah IBT dalam tempoh yang sama
|
Kad PK
|
NA
|
50%
|
26.9%
(75/279)
|
|
8.% IBT yang enggan menerima kaedah PK.
|
Bil IHBT yang enggan menerima kaedah PK
X 100
Jumlah semua kes IBT
|
Kad KIK 1(b)/96
|
34.2
|
20
|
2.6%
(12/453)
|
|
9. % suami IBT yang enggan memberi keizinan kepada
isteri untuk mengamalkan PK
|
bil suami kpd isteri IBT yang tidak izin isteri
mengamalkan PK
x
100
|
Kad KIK 1(b)/96
|
2.18%
|
0%
|
0%
|
3.
DIFFICULTY INDICATOR
|
1. IBT yang mendaptakn kaedah PK yang dibekalkan
oleh swasta atau dibeli terus dari kaunter farmasi
|
kaedah PK yang dibekalkan oleh swasta atau dibeli
dari farmasi x
100
Jumlah IBT dalam tempoh sama
|
Reten dari swasta atau farmasi
|
NA
|
20%
|
NA
|
11.0 PENCAPAIAN AKTIVITI YANG DIJALANKAN
|
ISU
|
STRATEGI
|
AKTIVITI
|
PENCAPAIAN
|
|
1.
Kurang pengetahuan dalam pengendalian PK untuk IBT
|
Meningkatkan
pengetahuan ibu melalui kaedah pendidikan kesihatan dan
penyeliaan berkesan
|
- Kursus /
latihan dalam perkhidmatan
-
Pengendalian PK
-
kemahiran IUCD
insertion
- Clinical
Nursing education
- case
study
- Penyeliaan
berkesan semasa sessi PK
- laporan
penyeliaan mengikut format penyeliaan
- Kajian
mengenai pengetahuan IBT mengenai PK
|
2
Kursus dijalankan melibatkan 60 anggota kejururawatn
3
orang Dr telah menjalani kemahiran IUCD insertion dgn FMS
dan sesama mereka
3
kes study dijalankan
45
penyeliaan berkesan dijalankan di KK dan KD
Kajian
pengetahuan ibu dijalankan 2 kali
|
|
2.Kelemahan
pengendalian PK kpd IBT
|
Meningkatkan
pengendalian kes dan keciciran secara berkesan melalui
pengesanan keciciran dalam masa 48 jam
|
- Mengenalpasti
kes keciciran selepas sessi klinik
- Menjalankan
pengesanan keciciran melalui telefon atau lawatan ke
rumah
- Kaunseling
kepada ibu dan keluarga
- Semakan
kad PK semasa penyeliaan
|
Kes
dikenalpasti selepas
sessi klinik 100%
Pengesanan
dijalankan selepas tercicir 1 minggu
Sessi
kaunseling dijalankan – individu (79 kali)
Semakan
kad dilakukan semasa penyeliaan
|
|
U
|
STRATEGI
|
AKTIVITI
|
PENCAPAIAN
|
|
3.
Kurang pilihan kaedah PK
|
Memastikan
pilihan kaedah PK yang mencukupi
|
- Memastikan
anggaran peruntukan dilakukan pada awal tahun
- Pesanan
dilakukan untuk bekalan yang mencukupi bagi 1 tahun
- Semakan
stok pada setiap bulan
- Pendidikan
kesihatan mengenai kaedah PK yang sediada kepada IBT
- Ceramah
- focus
group discussion (79)
|
1.
Anggaran peruntukan dilakukan pada awal tahun tetapi
masalah bekalan dari pembekal
2.
Pesanan dilakukan mengikut penggal
3.
Semakan stok dilakukan setiap bulan mengikut reten dan
baki fizikal
4.
FGD yang dilakukan : 79 sessi
|
|
4.
Ibu tidak komplians kepada kaedah PK
|
Meningkatkan
komplians ibu kpd PK melalui pendidikan kesihatan berkesan
dan kaunseling serta membetulkan kepercayaan dan
mispersepsi mengenai PK
|
- Promosi
kesihatan yang berkesan kepada IBT
- ceramah
kesihatan pada 36 minggu untuk IBT
- kaunseling
semasa postnatal
- FGD
kepada ibu dan suami
- pamphlet
kepada ibu semasa sessi ceramah
- Kajian
mengenai pengetahuan anggota mengenai aspek PK dan
pengendalian kes PK
|
- Ceramah
pada 36 minggu kandungan ke atas - 208 org diberi
ceramah
- Kaunseling
semasa postnatal - 435 orang
- FGD sessi
– 79 sessi
- pamphlet
diberikan kepada ibu
- Kajian
pengetahuan mengenai pengetahuan anggota mengenai
aspek PK dan pengendalian kes dilakukan 2 kali.
|
12.
PERBINCANGAN
Masalah
kurang pengamalan perancang keluarga di kalangan IBT telah
dipilih sebagai masalah yang perlu ditangani dengan segera dan
berkesan. Ini ialah kerana IBT perlu diberikan pilihan untuk
merancang kehamilan mereka agar keadaan berisiko mereka akan
pulih sebelum kehamilan akan datang.
Keadaan
seperti anaemia semasa mengandung banyak dipengaruhi oleh
keadaan ibu yang kerap mengandung, pemakanan tidak seimbang atau
masalah perubatan seperti thalassemia atau thalassemia trait.
Keadaan ini akan pulih apabila iron reserve kembali ke normal
apabila ibu menjarakkan kandungannya. Walaupun kehamilan adalah
perubahan fisiologik dan bukan keadaan yang patologik tetapi
jika tidak ditangani dengan baik, ia akan mengakibatkan keadaan
yang memudaratkan ibu dan anak.
Amalan
perancang keluarga dengan kaedah yang ada di Kemudahan
Kementerian Kesihatan membantu proses kehamilan yang terancang
dan dengan itu menjamin keadaan ibu dan bayi yang sihat.
Terdapat pelbagai kaedah yang boleh didapati di KK dan KD
seperti IUCD, suntikan unidepo, pil kontraseptif dan kondom.
Perancangan untuk membeli peralatan ini dilakukan setiap awal
setiap tahun dan inden dilakukan secara penggal.
Dari
kajian awal ke atas IBT mendapati kebanyakan ibu adalah Melayu,
berumur antara 20 -34 tahun, berpendidikan sekolah menengah,
pariti 2 – 5 dan mempunyai pendapatn antara RM1501 – RM 2500
sebulan. 54.6% pernah mengamalkan perancang keluarga dan kaedah
yang paling popular ialah pil (50.9%). Kaedah ini dipilih kerana
ia merupakan kaedah yang paling mudah (54.6%). Penggalak utama
kepada amalan perancang keluarga ialah kakitangan kesihatan
iaitu 57.5%. Terdapat 7.5% suami yang tidak yakin dan tidak
bersetuju dengan kaedah perancang keluarga moden. 79.6% IBT
mempunyai tag bewarna kuning dan selebihnya mempunyai tag merah.
Faktor risiko yang paling utama ialah PIH iaitu 42.6% diikuti
dengan anaemia iaitu 16.7%. Hanya 37% ibu dapat memberikan 5
kaedah perancang keluarga yang ada di KKM. 49.1% dari IBT
mendapat pengetahuan mengenai perancang keluarga dari kakitangan
kesihatan dan 85% dari mereka mendapatkannya dari Klinik
kerajaan atau swasta.
17
respond menyatakan mereka tidak amal perancang keluarga kerana
khuatir berat badan bertambah dan 8 respond mempunyai masalah
sakit kepala. Jika tidak mengamalkan perancang keluarga, 97.4%
memberi respond mereka akan mengandung. 25.9% menyatakan masalah
kegemukan adalah kesan sampingan buruk setengah kaedah perancang
keluarga (PK).
Dari
skor kajian ini mendapati bahawa 66.6% dari ibu mendapat markah
60% - 80% skor dan hanya 7.4% mendapat skor melebihi 80%.
Kajian pengetahuan kakitangan mengenai pengetahuan
mengenai PK dan pengendalian PK mendapati hanya 1 (1.7%)
mendapat skor melebih 80% tetapi setelah kursus, didapati bahawa
86.7% (52) mendapat skor melebih 80%.
Ceramah
mengenai PK diberikan sejak booking dan diperkukuhkan pada 36
minggu kandungan. Semasa 36 minggu ke atas ibu diminta membuat
pilihan kaedah PK. Pada lawatan postnatal sekali lagi ia
diperkukuhkan tetapi jika hubungan seksual bermula lebih awal
dari pilihan kaedah PK, ini akan mengakibatkan ibu menghadapi
risiko mengandung. Dari data yang diperolehi, didapati bahawa
579 dari 599 IBT yang diberikan pendidikan kesihatan mengenai PK
telah bersetuju untuk mengamalkan PK. Sejumlah 79 sessi FGD
telah dilakukan dan 77 (97.5%) ibu bersetuju untuk mengamal PK
selepas sessi FGD tetapi hanya 59% (269) sahaja yang benar-benar
mengamalkannya.
Sessi
ceramah dan FGD diberikan kepada ibu dan suami untuk membantu
mereka dalam membuat keputusan. 79 sessi FGD telah dijalankan
dari Januari – Jun 2004. Sessi kaunseling individu juga
dijalankan semasa lawatan postnatal.
Jelas
sekali bahawa pengetahuan dan keputusan untuk mengamalkan kaedah
PK boleh berubah oleh faktor-faktor lain. Sessi latihan juga
telah dijalankan kepada anggota kejururawatan untuk meningkatkan
kemahiran mereka mengendalikan sessi PK di KK atau KD.
Setelah
menjalankan semua aktiviti ini, indikator kesihatan telah dapat
ditingkatkan dari 45.8% ke 61.1% (279/453) dan tiada kematian
ibu IBT yang tidak amalkan PK.
Masih
banyak perlu dilakukan terutama memperkukuhkan mengenai
pendidikan kesihatan dan salahanggap mengenai PK seperti masalah
kenaikan berat badan, pening, muntah dan kesan sampingan lain.
Jika terdapat kesan sampingan terdapat kaedah lain yang tidak
menggunakan hormon yang boleh disyorkan kepada ibu. Keputusan
untuk mengambil atau tidak masih di tangan ibu walaupun
kebanyakan ibu mendapat maklumat dari anggota di KK dan KD.
Keciciran
ibu dari klinik PK perlu diambil tindakan pengesanan segera
untuk mengelakkan ibu lalai dan tidak menggunakan kaedah PK yang
telah dibekalkan. Keciciran juga mungkin bermakna ibu mengalami
kesan sampingan dan perlu memberikan nasihat supaya mereka
menukar kepada kaedah lain yang tiada kesan sampingan. Amalan PK
selama 6 bulan merupakan indikator kesungguhan ibu dalam
mengambil kaedah PK yang disyorkan.
Masih terdapat 2.6% IBT yang enggan menerma kaedah PK
yang telah disyorkan tetapi 0% dari suarmi yang tidak benarkan.
- KESIMPULAN
Aktiviti
yang telah dijalankan telah berjaya meningkatkan amalan PK di
kalangan IBT dari 45.8% kepada 61.6%. Ia masih jauh dari sasaran
yang ditetapkan. Pendidikan kesihatan mengenai PK masih tidak
mencapai 100% seperti disasarkan. Keciciran dari sessi PK perlu
diambil tindakan untuk pengesanan untuk mengelakkan mereka
berhenti menggunakan kaedah PK yang telah digunakan.
Laporan
disediakan oleh:
Dr.Hajjah
Hayati Mohd Radzi
Pegawai
Kesihatan Daerah Pendang
Dibantu
oleh:
KJK
Ishah Rashid
KJK
Maimunah Md. Noor
***********************************************************************
PROJEK
INOVASI
EAS
2000
(EPID AUTO SPOT 2000)
SEBUAH
PETA MAYA YANG BERFUNGSI SECARA INTERAKTIF DAN DAPAT MENGHASILKAN
INFORMASI EPIDEMIOLOGI DENGAN PANTAS
PePendahuluan
Dalam
pengurusan Kesihatan Awam, aspek survaillance dan pencegahan
penyakit merupakan tonggak utama yang dijalankan. Berbagai cara
telah dipraktikkan dalam menjalankanaktiviti tersebut seperti
penyimpanan rekod dalam buku rekod besar, reten-reten,
laporan-laporan dan sebagainya.
Bagaimana pun, dalam era IT ini, cara-cara yang dipraktikkan
sekarang boleh dipertingkatan lagi dengan bantuan komputer dalam
beberapa aspek supaya ianya menjadi lebih mudah, ringkas, kemas
dan efektif serta dapat dimanafaatkan oleh semua kategori anggota
kesihatan.
2.
Rationale
2.1.
Situasi Semasa
Mengikut cara penyimpanan rekod yang diamalkan sekarang,
maklumat-maklumat yang didapati seperti maklumat kes, maklumat
rawatan, maklumat kontak, sosiodemografi dan lain-lain lagi akan
direkodkan pada buku rekod atau peta kawasan operasi secara
manual. Bagi menganalisa atau membuat surveillance kejadian
sesuatu penyakit bagi tujuan membuat tindakan bersepadu yang lain
seperti kawalan berkala, ACD dan pendidikan kesihatan, ianya agak
rumit kerana rekod-rekod tersebut tidak begitu nyata tentang
kedudukan kes–kes diseluruh daerah Pendang. Ianya mungkin
terpaksa disemak dari beberapa rekod dan fail yang berlainan untuk
mendapat maklumat yang lengkap. Kaedah ini tidak kemas, boleh
hilang dan sukar untuk mendapt maklumat yang lebih terperinci
dalam masa yang singkat.
2.2.
Sistem yang dicadangkan
Menyedari
hakikat ini, anggota
dari Pejabat Kesihatan Daerah Pendang telah cuba untuk
mengwujudkan satu sistem yang lebih sistematik, mudah serta cepat
untuk mengesan kedudukan setiap kes dengan semua data berkaitankes
dipaparkan secara multimedia.
Memandangkan kejadiana kes TIBI merupakan antara masalah kesihatan
utama di daerah Pendang dimana kadar insidennya merupakan antar
yang tertinggi di negeri Kedah, maka satu sistem surveilance yang
lebih mudah dan lengkap diperlukan bagi merangka strategi
pencegahan dan kawalan penyakit tersebut.
Dengan
terciptanya “Epid Auto Spot 2000’ (EAS2000), kedudukan serta
maklumat kes dapat diperolehi
dan dilihat serta merta tanpa perlu membelek beberapa fail.
Adalah diharapkan dengan adanya EAS 2000 ini, diharapkan program
surveillance akan dapat ditingkatkan dan diperkemaskan lagi dan
seterusnya memberi kesan yang lebih positif kepada program-progran
kawalan dan pencegahan. Memandangkan EAS 2000 agak mudah untuk
dipelajari dan difahami, maka dirasakan lebih banyak unit dapat
menggunakan sistem ini termasuk
MCH, BAKAS dan lain-lain.
3.
Objektif
3.1. Objektif Umum
Mewujudkan
satu sistem surveillance kejadian penyakit berjangkit menggunakan
multimedia supaya memudahkan aktiviti kawalan dan pencegahan dapat
dijalankan dengan lebih cepat dan tepat.
3.2.Objektif Khusus
3.2.1.
Bagi mengenalpasti kedudukan kes-kes penyakit diseluruh
daerah Pendang.
3.2.2.
Memudahkan proses penyemakan maklumat pesakit dimana
maklumat dapat diperolehi pada skrin yang sama dengan skrin yang
menunjukkan kedudukan pesakit pada peta.
3.2.3.
Mengenalpasti faktor sosiodemografi untuk setiap kes bagi
membuat persediaan yang bersesuaian untuk tindakan kawalan dan
pencegahan.
3.2.4.
Menggalakkan/memahirkan Anggota Kesihatan dengan penggunaan
IT dalam kerja seharian.
3.2.5.
Mengurangkan kos dan menjimatkan masa kerana maklumat yang
direkodkan dapat diperolehi dengan serta-merta apabila dikehendaki.
4. Metodologi
Masalah
utama yang sering timbul didalam menjalankan aktiviti kawalan dan
pencegahan penyakit berjangkit adalah berkaitan pengurusan data
mengenai kes, kontak, maklumat klinikal, faktor sosiodemografi dan
lain-lain yang mana selalunya hanya direkodkan dalam buku rekod
dan fail-fail tertentu. Melalui kaedah ini kita tidak dapat
melihat dengan jelas kedudukan kes, maklumat-maklumat kes ataupun
hubungan dengan kes lain dimana maklumat asas ini sangat
diperlukan untuk menjalankan aktiviti pencegahan dan kawalan.
Sehubungan
itu, satu pasukan telah dibentuk yang mana terdiri dari IK CDC,
dan sebilangan PKA bagi membincang, mengenalpasti masalah dan cuba
mencari kaedah terbaik bagi menyelesaikan masalah tersebut.
Didapati
satu kaedah yang sering dipraktikkan di bilik gerakan semasa
kejadian sesuatu wabak penyakit iaitu peta lokasi (selalunya peta
daerah) yang menunjukkan kedudukan kes sesuai digunakan untuk
projek ini. Dengan kaedah ini ‘map pin’ akan dicucuk diatas
peta bagi menandakan kedudukan setiap kes. Tetapi, pada
kebiasaannya hanya nama-nama kes sahaja dipamerkan pada peta
tersebut. Maklumat-maklumat lain berkenaan kes seperti maklumat
klinikal, kontak, sosiodemografi dan lain-lain tidak dapat
dipamerkan pada peta tersebut kerana keadaan ini akan menyebabkan
peta itu kelihatan terlalu padat dan berserabut.
Setelah
mengetahui permasalahan asas, tugasan utama adalah bagaimana
menyediakan satu peta yang dapat menunjukkan kedudukan kes dan
juga mempunyai segala butir-butir lengkap mengenai kes dengan
kemas tanpa berselerak diatas peta tadi. Akhirnya, setelah
beberapa percubaan dijalankan,
sebuah peta maya (EAS 2000) yang berkonsepkan intraktif dan
dapat memenuhi segala aspek yang dibincangkan telah dihasilkan
dengan menggunakan perisian Macromedia Authorware Professional
Attain 5.
5. Perlaksanaan
Sebuah
peta daerah Pendang dipaparkan pada skrin komputer dengan ditanda
bulatan-bulatan putih kecil bagi mewakili kedudukan kes-kes TIBI
di seluruh daerah Pendang. Di peta itu juga dipaparkan keadaan
geografi daerah. Segala maklumat mengenai setiap kes dimasukkan
tetapi pada program ini tetapi tidak kelihatan pada skrin komputer.
Hanya apabila cursor diklik diatas penanda kedudukan kes diatas
peta, maklumat berkenaan kes tersebut akan dipaparkan dengan serta
merta. Dengan kaedah ini, banyak penanda kedudukan kes boleh
diletakkan diatas peta tersebut tanpa membuatkan ianya nampak
penuh dan berserabut.
Semua
maklumat mengenai kes, kontak, klinikal, sosiodemografi dan
lain-lain boleh didapati pada satu paparan skrin komputer sahaja
dengan serta merta. Dengan ini,
persediaan untuk membuat langkah-langkah kawalan dan
pencegahan dapat disediakan dengan lebih teratur dan sempurna
berdasarkan maklumat-maklumat yang dipaparkan.
6. Kesimpulan
EAS
2000 dihasilkan bersesuaian dengan seruan kerajaan agar semua
jabatan lebih melibatkan bidang IT bagi membantu kerja seharian.
ESM 2000 dicipta dengan harapan dapat membantu memudahkan
urusan-urusan survaillance, pencegahan dan kawalan didalam program
Kesihatan Awam. Selain dari memudahkan, ianya juga membolehkan
kerja-kerja dilakukan dengan lebih cepat, kemas dan effisien
berbanding cara lama yang terpaksa menyemak rekod-rekod yang
ditulis di kertas, sekali gus dapat meningkatkan produktiviti
jabatan serta mengurangkan kos operasi. Disamping itu, ianya juga
dapat mendorong kakitangan Kesihatan lebih memahirkan diri dengan
dunia IT.
7. Cadangan Penambahbaikan
EAS 2000 yang
menggunakan aplikasi program Macromedia Authorware Profesional
Attain 5 senang dipelajari, difahami dan digunakan. Segala
penambahan maklumat yang difikirkan perlu senang untuk
dilaksanakan. Sebagai contohnya, penambahan maklumat-maklumat
Klinik Desa pada peta daerah Pendang. Apabila diklik pada penanda
klinik di peta tersebut, satu paparan yang mengandungi semua
maklumat mengenai klinik tersebut seperti JM yang menyelia,
liputan kawasan operasi dan lain-lain akan muncul diskrin.
Cadangan
pada masa depan, EAS 2000 akan dimajukan lagi dengan menambahkan
semua maklumat daerah seperti bilangan penduduk, jumlah liputan
BAKAS( air bersih, tandas, air limbah dll), bilangan kedai makan/restoren,
bilangan kilang dan sebagainya hanya dalam satu skrin.
Maklumat
pesakit akan terpapar disebelah kanan (kotak biru) apabila diklik
pada bulatan putih diatas peta yang mewakili kedudukan kes.
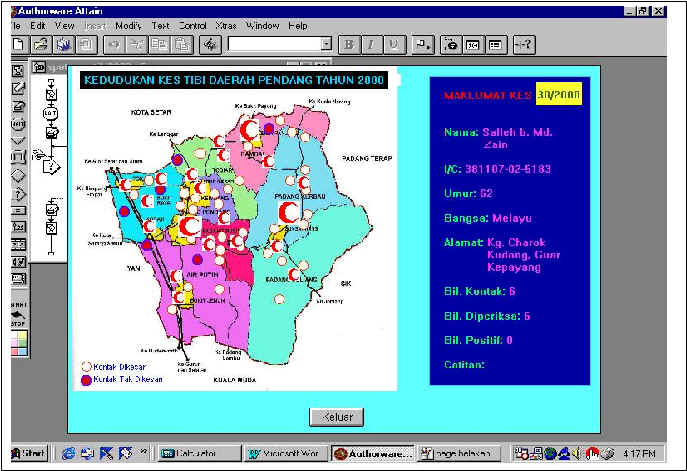
|